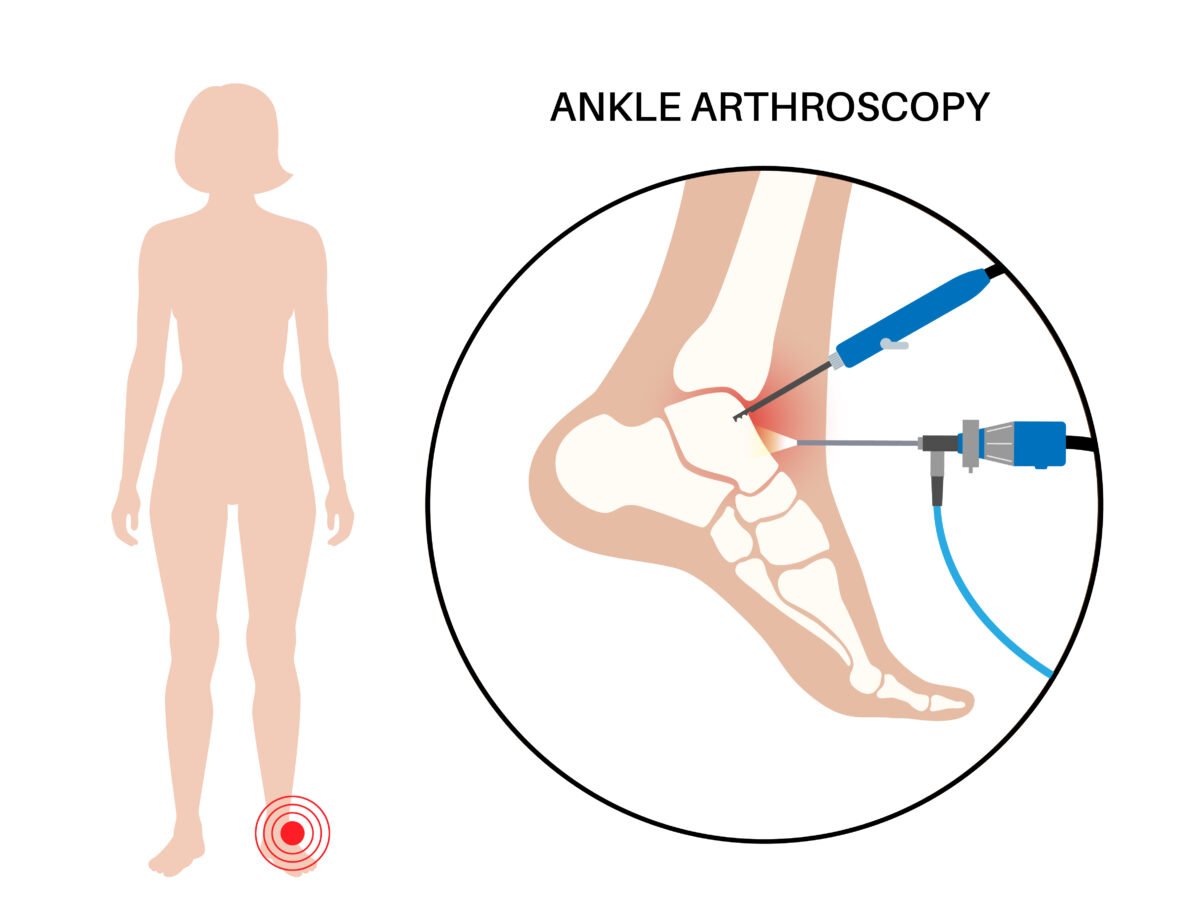
Ankle arthroscopy is very common and surgeons are able to treat more conditions than ever before thanks to recent technological advances. Arthroscopy is becoming a standard procedure as surgeons are able to perform increasingly complex procedures with less invasive methods and lower risks.
ΑΡΘΡΑ

Wrist arthroscopy can be used to diagnose and treat many conditions, including wrist tissue injuries, carpal arthritis, tendon tears, osteochondrosis, and other problems. The surgeon can examine the condition of the tissues, cartilage, and joints of the wrist and perform necessary procedures, such as removal of detached particles, bone or tendon repair, and cartilage repair.
What are the indications for elbow arthroscopy?
Some of the main indications for wrist arthroscopy include:
- Wrist Arthritis: Arthroscopy can be helpful in diagnosing and treating wrist arthritis, which can cause pain, swelling, and limited mobility.
- Cartilage Rupture: Arthroscopy is used to repair tears or damage to the cartilage in the wrist.
- Carpal Coexistence of Free Particles: If there are free particles or small pieces of cartilage in the wrist, arthroscopy can be used to remove them.
- Carpal Rib Coexistence: In cases of tendon tears, such as extensor carpi ulnaris or flexor carpi ulnaris, arthroscopy can be used for repair.
- Carpal Coexistence of Tendonitis or Tendinopathy: Problems with the carpal tendons, such as tendinitis or tendinopathy, can be treated with arthroscopic techniques.
The choice of wrist arthroscopy depends on the type and severity of the problem, as well as the general condition of the patient. The surgeon will take these parameters into account when determining the appropriate treatment plan.
Arthroscopic surgical treatment of the wrist

Arthroscopic surgery can be used to treat certain wrist conditions, including but not limited to:
- Chronic wrist pain. Arthroscopic exploratory surgery can be used to diagnose the cause of chronic wrist pain when the results of other tests do not provide a clear diagnosis. Often, there may be areas of inflammation, cartilage damage, or other findings that explain the pain. In some cases, after diagnosis, the condition can also be treated arthroscopically — and possibly during the same procedure.
- Wrist fractures. Small fragments of bone may remain in the joint after a bone is broken (fractures). Wrist arthroscopy can be used to remove these fragments and realign the broken pieces of bone. The bone is then fixed using pins, wires, screws, plates, etc.
- Ganglion cysts. Ganglion cysts usually develop outside the joint from a stalk between two of the carpal bones. Usually, the cyst and/or its stalk can be seen and removed during arthroscopy, eliminating the cyst.
- Ligament/triangular fibrocartilage complex (TFCC) tears. Ligaments are fibrous bands of connective tissue that connect bones together. They provide stability and support to the joints. The TFCC is a structure that stabilizes and softens the wrist. A fall on an outstretched arm (eg, from slipping on an icy surface or while participating in sports) can injure or tear ligaments in the wrist, such as the TFCC. This can cause wrist pain, especially during activity. Arthroscopic surgery can be used to diagnose and treat TFCC and other wrist ligament tears.

Elbow arthroscopy has proven to be extremely effective in treating a variety of conditions and conditions. This method allows the surgeon to examine the condition of the soft tissues, bones and joints of the elbow with great precision. Through the arthroscope, doctors can confirm diagnoses and assess the severity of elbow problems, such as cartilage injuries, tendinitis, sprains, tears, and arthritis.
One of the major advantages of elbow arthroscopy is the minimal intervention on the surrounding tissues. The small incisions required to insert the arthroscope allow minimal scarring and minimize pain and recovery time. Also, patients who undergo arthroscopic elbow surgery usually recover elbow mobility and function more quickly compared to open surgery.
Overall, elbow arthroscopy is an advanced technique that offers accurate diagnosis and effective treatment for many elbow problems. If you are experiencing problems with your elbow, it is recommended that you speak with a specialist surgeon about applying this advanced technique that can provide you with the relief and rehabilitation you need.
What are the indications for elbow arthroscopy?
Indications for elbow arthroscopy include a variety of conditions that affect the elbow and can be treated with this surgical technique. Key indications include:
- Traumatic Conditions: Tendon sprains and conditions caused by accidents may require arthroscopy for diagnosis and treatment.
- Chronic Degenerative Arthritis: Osteoarthritis or rheumatoid arthritis that causes chronic pain and cartilage wear can be treated with arthroscopic techniques.
Procedure
During the operation, the surgeon examines the structures of the elbow. It can then perform various procedures, such as tendon repair, cartilage repair, and free particle removal.
When is elbow arthroscopy recommended?

Your doctor may recommend elbow arthroscopy if you have a painful condition that doesn’t respond to nonsurgical treatment. Nonsurgical treatment includes rest, physical therapy, and medications or injections that can reduce inflammation. Inflammation is one of your body’s normal responses to injury or illness. In an injured or diseased elbow joint, inflammation causes swelling, pain and stiffness.
Injury, overuse, and age-related wear and tear are responsible for most elbow problems. Elbow arthroscopy can relieve the painful symptoms of many problems that damage the cartilage surfaces and other soft tissues surrounding the joint. Elbow arthroscopy may also be recommended to remove loose pieces of bone and cartilage or to release scar tissue that prevents movement.
Common arthroscopic procedures include:
- Treatment of lateral elbow epicondylitis
- Removal of loose bodies (loose cartilage and bone fragments)
- Release scar tissue to improve range of motion
- Treatment of osteoarthritis (wear and tear arthritis)
- Treatment of rheumatoid arthritis (inflammatory arthritis)
- Treatment of osteochondritis (activity-related damage to the head of the humerus seen in female athletes)
- Treatment of fractures
The video belongs to the channel MotionLit

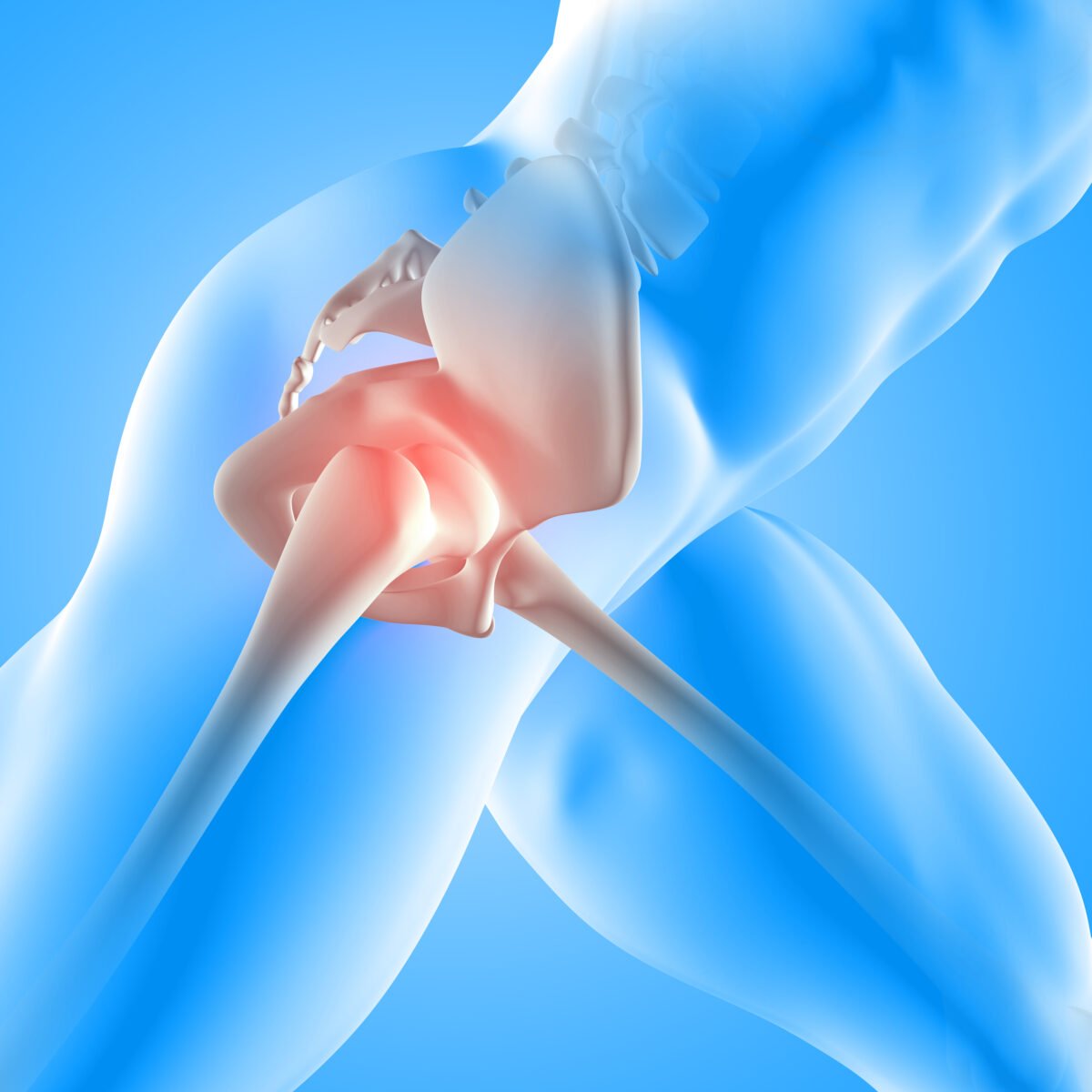
What is Total Hip Arthroplasty?
Total hip arthroplasty, commonly known as hip replacement surgery, is a medical procedure designed to relieve hip pain and improve function in patients with severe hip joint damage. This damage can result from various conditions such as osteoarthritis, rheumatoid arthritis, fractures, or other degenerative joint diseases.
Why is Total Hip Arthroplasty Needed?
The hip joint is a ball-and-socket joint, where the ball (femoral head) fits into the socket (acetabulum) of the pelvis. Over time, the cartilage that cushions these bones can wear away, leading to pain, stiffness, and reduced mobility. When conservative treatments like medications, physical therapy, and lifestyle modifications fail to alleviate symptoms, total hip arthroplasty becomes a viable option.
The Procedure
During total hip arthroplasty, the surgeon removes the damaged bone and cartilage and replaces them with artificial components:
- Femoral Component: A metal stem is inserted into the thigh bone (femur), and a metal or ceramic ball is placed on the upper part of the stem.
- Acetabular Component: The damaged socket is replaced with a metal socket, which may also have a plastic, ceramic, or metal liner to allow smooth movement.
Types of Hip Implants
- Cemented Implants: These use a special bone cement to secure the implants to the existing bone.
- Uncemented Implants: These rely on bone growth to secure the implant, often having a porous surface that encourages natural bone to grow into it.
- Hybrid Implants: A combination of cemented and uncemented components.
Benefits of Total Hip Arthroplasty
- Pain Relief: The primary benefit is the significant reduction or elimination of hip pain.
- Improved Mobility: Patients typically experience enhanced movement and flexibility, allowing them to return to daily activities and enjoy a better quality of life.
- High Success Rate: Hip replacement surgeries have a high success rate, with many patients experiencing long-term relief and improved joint function.
Recovery Process
Recovery from total hip arthroplasty involves several stages:
- Hospital Stay: Patients usually stay in the hospital for a few days post-surgery. During this time, pain management and early mobilization are key focuses.
- Physical Therapy: A structured physical therapy program is essential for regaining strength and mobility. Therapists guide patients through exercises to improve hip function and prevent complications.
- At-Home Care: Once discharged, patients must follow specific guidelines to protect the new hip joint, including avoiding certain movements and positions.
- Follow-Up Appointments: Regular follow-up visits with the surgeon ensure proper healing and monitor for any potential issues.
Risks and Complications
As with any surgical procedure, total hip arthroplasty carries potential risks, including:
- Infection: Though rare, infections can occur around the artificial joint.
- Blood Clots: Measures such as blood-thinning medications and exercises are used to minimize this risk.
- Dislocation: Proper post-surgical care and adherence to movement restrictions reduce this risk.
- Implant Wear and Tear: Over time, artificial components can wear out, potentially requiring revision surgery.
The video belongs to Arthrex

Three different types of pain relief (anesthesia) may be used for knee arthroscopy surgery:
- Local anesthesia. Your knee may be numbed with pain medicine. You may also be given medication to relax you. You will stay awake.
- Spinal anesthesia. This is also called regional anesthesia. Pain medicine is injected into a space in your spine. You’ll be awake but won’t be able to feel anything below your waist.
- General anesthesia. You will be asleep and pain free. Peripheral nerve block (femoral or afferent canal block). This is another type of regional anesthesia. Pain medicine is injected around the nerve in your groin. You will be asleep during the operation. This type of anesthesia will block pain so you need less general anesthesia.
A device may be placed around your thigh to help control bleeding during the procedure. The surgeon will make 2 or 3 small incisions around your knee. Fluid (saline) will be pumped into your knee to inflate the knee.
A narrow tube with a tiny camera on the end will be inserted through one of the cuts. The camera is connected to a video monitor that allows the surgeon to see inside the knee. The surgeon can put other small surgical tools into your knee through the other cuts. The surgeon will then correct or remove the problem in your knee.
At the end of your surgery, saline will be drained from your knee. The surgeon will close your incisions with stitches (stitches) and cover them with a bandage. Many surgeons take pictures of the procedure from the video monitor. You may be able to view these images after surgery so you can see what was done.
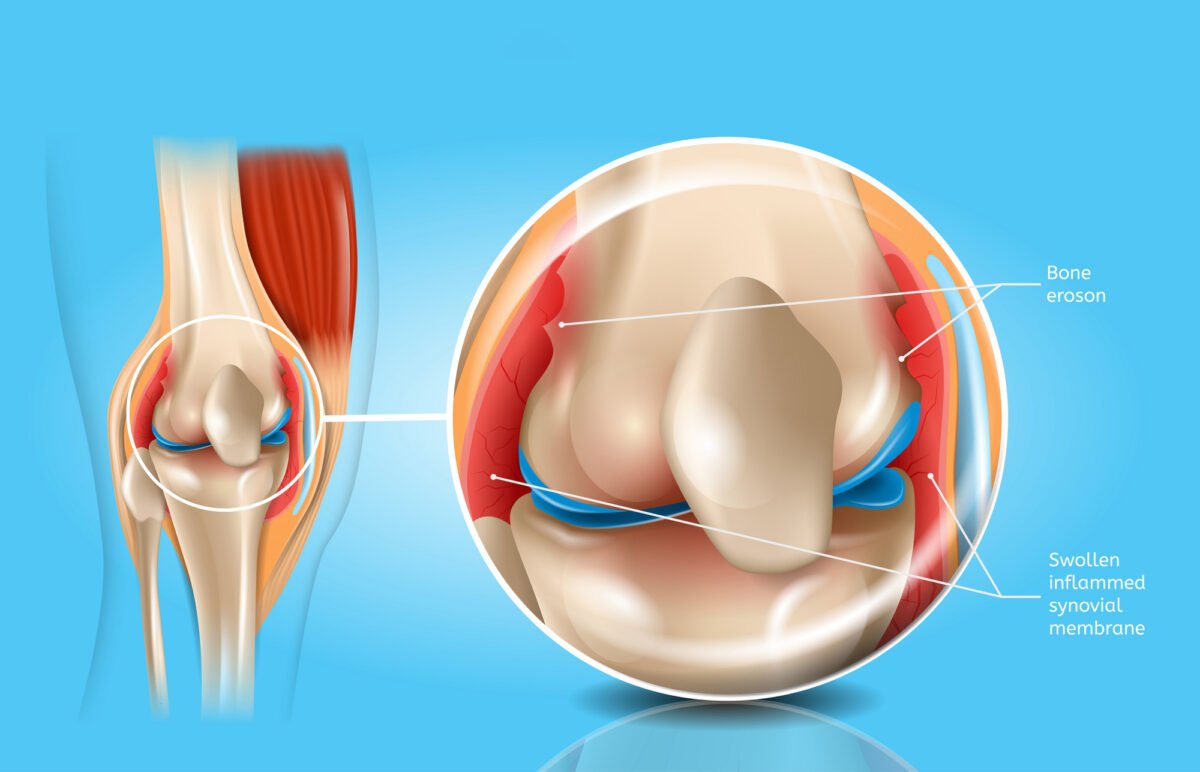
Why is knee arthroscopy performed?
Arthroscopy may be recommended for these knee problems:
- Torn meniscus. The meniscus is cartilage that covers the space between the bones in the knee. Surgery is done to repair or remove it.
- Torn or damaged anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL).
- Swollen (inflammation) or damaged lining of the joint. This lining is called the synovium.
- Patella (patella) that is out of position (misalignment).
- Small pieces of broken cartilage in the knee joint.
- Baker cyst removal. This is a swelling behind the knee that is filled with fluid. Sometimes the problem occurs when there is swelling and pain (inflammation) from other causes, such as arthritis.
- Cartilage defect repair.
- Some fractures of the knee bones.
What is the success rate of knee arthroscopy?

The success rate of knee arthroscopy has steadily increased over the years, with more recent studies reporting an overall success rate of approximately 85%. However, there are still some factors that can affect the success rate of this procedure and these vary from patient to patient. In general, though, the success rate for knee arthroscopy is very high when performed by experienced surgeons.
Well, in patients over 50, the success rate of knee arthroscopy is about 71%. However, in younger patients under the age of 50, the success rate is about 87%. This is mainly because younger patients tend to have more bone formation in the knee joint. This means that their knee cartilage tends to be more developed and this can make surgery more difficult.
Factors affecting the success rate of knee arthroscopy?
There are many factors that affect the success rate of knee arthroscopy, including the patient’s age, health status, and surgical technique. Arthroscopic techniques have improved dramatically in recent years, so the success rate of this operation has also improved. However, there is still variation among surgeons in how successful they are in achieving these goals.
- Age: As the patient’s age increases, the success rate for knee arthroscopy decreases. This is because elderly patients are more likely to have osteoarthritis or other joint conditions that make arthroscopic surgery difficult.
- Health status: Patients with certain health conditions may be at higher risk for complications during the procedure. For example, patients with heart disease or diabetes are at high risk for an adverse outcome after knee arthroscopy.
- Process technique: The technique that the surgeon uses can affect the success rate of arthroscopic surgery. A small percentage of surgeons perform arthroscopic surgery using an endoscope, while others use cameras and robotic arms to remove debris from the knee joint.
How has the success rate of knee arthroscopy surgery changed over time?
The success rate of knee arthroscopy surgery has steadily increased over the years due to new technology and improved surgical techniques. In 2000, the success rate was only 60%. However, by 2014, the success rate had risen to 86%. This increase is believed to be due to improvements in surgical techniques, more experienced surgeons and better equipment.
Knee arthroscopy with endotherapy
Knee arthroscopy with endotherapy is an advanced medical procedure used to diagnose and treat knee problems. It is one of the most effective means of treating injuries or diseases of the knee, offering at the same time shorter recovery times compared to traditional surgical methods.
Endotherapy, which means treatment inside the joint, may involve removing damaged tissue, repairing cartilage, or using special techniques such as repositioning certain structures. This operation can help relieve pain and improve knee mobility. This procedure is usually performed under local anesthesia, with a small incision in the knee to insert the arthroscope and instruments.
Knee arthroscopy with endotherapy is often an option for athletes or people who wish to quickly return to their daily activities. However, it is important to note that each case is unique and that the decision to implement this procedure should be made after discussion with an orthopedic specialist to ensure the appropriate approach and treatment.
During the process
The video belongs to the channel Silverback Video
Shoulder arthroscopy is a minimally invasive surgical procedure used to diagnose and treat problems inside the shoulder joint. It involves the use of a small camera called an arthroscope, which is inserted into the shoulder through small incisions.
Calcific tendinitis of the shoulder is a particularly painful condition resulting from the deposition of calcium salts in the tendon mass of the rotator cuff.
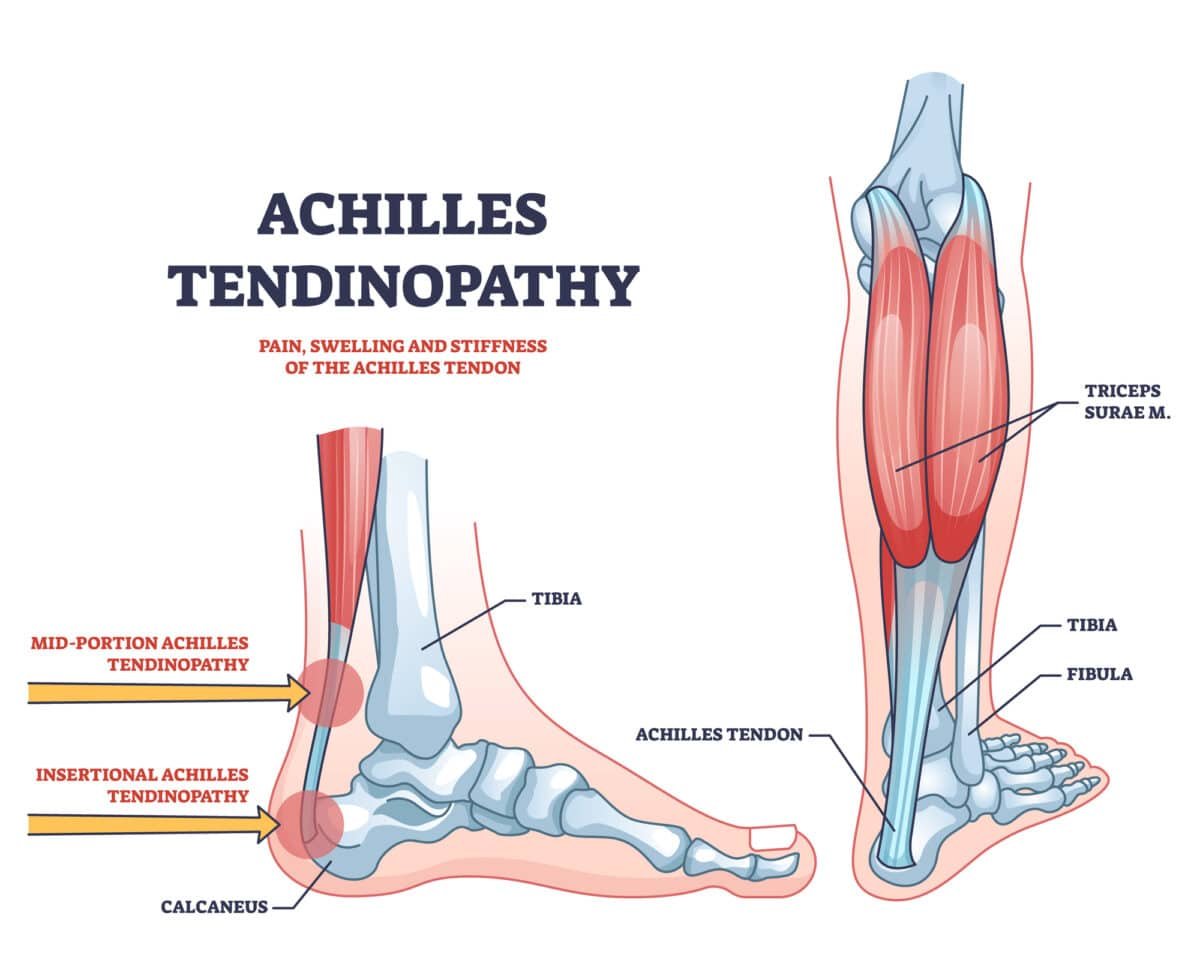
Achilles tendinitis is a common cause of pain in athletes. The predisposing factors of the condition include increased mechanical stress on the Achilles tendon, poor perfusion of the tendon 3-4 cm from its insertion, the use of fluoroquinolones as well as inflammatory arthropathies.