KNEE ARTHRITIS
Your joints are involved in almost every activity you do. Movements such as walking, bending and turning require the use of your hip and knee joints. When the knee becomes pathological or injured, the resulting pain can severely limit your ability to move and work. The knee is the largest joint in the body and plays a central role in almost every daily activity. The knee joint is formed by the ends of three bones:
- The lower end of the femur or thigh.
- The upper end of the tibia or tibia.
- The kneecap.
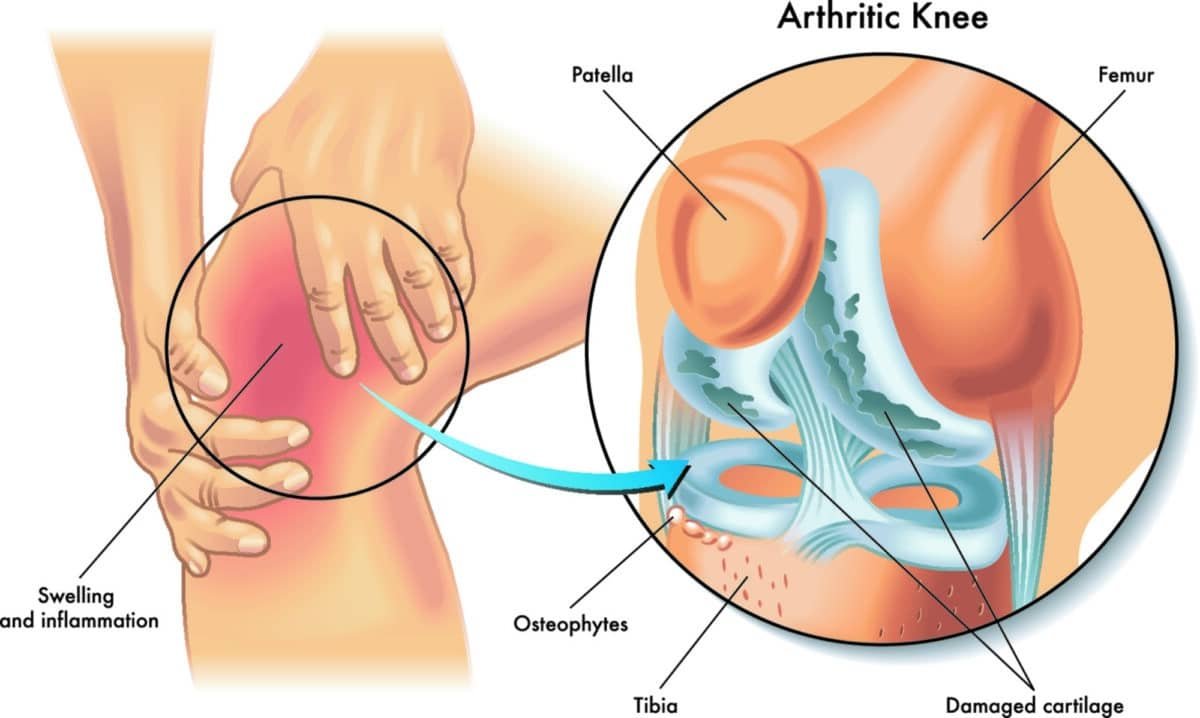
Thick tough bundles of tissue called ligaments connect the bones and stabilize the joint. A smooth coating with elastic properties called cartilage covers the ends of bones and prevents them from rubbing against each other, allowing flexible, nearly frictionless movement. Cartilage also absorbs shocks by protecting the bones from rubbing against each other. Finally, a soft tissue called the synovium covers the joint and produces a lubricating fluid that reduces friction and wear. Each patient is unique and may experience knee pain for different reasons.
A common cause of knee pain is osteoarthritis (OA). OA is sometimes called degenerative arthritis because it is a “wear and tear” condition that results in the cartilage in the joints wearing away. When the cartilage wears down, the bones rub against each other causing pain and stiffness.
Another common cause of knee pain is rheumatoid arthritis (RA). RA causes chemical changes in the joint cartilage, or synovium, resulting in thickening and inflammation. In turn, the synovial fluid destroys the cartilage. The end result is cartilage loss, pain and stiffness. If you haven’t gotten enough relief with conservative treatment options such as a brace, medication, or synovial fluid injection, your doctor may recommend total knee replacement.
Symptoms
A knee joint affected by arthritis can be painful. In general, pain develops gradually over time, although sudden onset is also possible. There are also other symptoms:
- The joint can become stiff and swollen, making it difficult to bend and straighten the knee.
- Pain and swelling may be worse in the morning.
- Strenuous activity can cause the pain to flare up.
- Loose fragments of cartilage and other tissue can interfere with joint movement. The knee may lock or stick during movement.
- The pain can cause a feeling of weakness in the knee.
- Many people with arthritis notice increased joint pain with the weather changes.
Examinations by the doctor
During your appointment, your doctor will talk with you about your symptoms and medical history, perform a physical exam, and possibly order diagnostic tests, such as X-rays or blood tests.
Prevention
Knee arthritis, a condition characterized by inflammation and degeneration of the knee joint, can significantly affect mobility and quality of life. While some risk factors for arthritis are out of your control, taking some preventative measures can help minimize your chance of developing knee arthritis:
- Maintain a healthy weight: Excess body weight puts extra stress on the knee joints. By maintaining a healthy weight through a balanced diet and regular exercise, you can reduce your risk of developing arthritis and relieve stress on your knees.
- Regular exercise: Engage in exercises that promote joint flexibility and strength, such as swimming, cycling and walking. These activities help maintain joint function and reduce the risk of arthritis.
- Protective equipment: If you participate in activities that pose a risk to the knees, such as contact sports or certain occupations, use appropriate protective equipment. This can help prevent injuries that can contribute to the development of arthritis.
- Proper posture and body mechanics: Maintain good posture and practice proper body mechanics, especially when lifting heavy objects or performing repetitive tasks. This reduces unnecessary stress on the knees.
Treatment
If knee arthritis has already developed, various treatment options aim to relieve pain, improve joint function and improve overall quality of life. Here are the key components of knee arthritis treatment:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), pain relievers, and corticosteroid injections are often prescribed to manage the pain and inflammation associated with knee arthritis.
- Physical therapy: A customized exercise program designed by a physical therapist can help strengthen the muscles around the knee, improve joint flexibility, and improve overall mobility.
- Lifestyle modifications: Adopting a supportive lifestyle, including weight management, low-impact exercises, and the use of assistive devices, can contribute to better knee health.
- Joint injections: In some cases, hyaluronic acid or platelet-rich plasma (PRP) injections may be considered to provide temporary relief and promote joint lubrication.
- Surgery: In advanced cases, surgeries such as arthroscopy, joint realignment, or knee replacement may be recommended to treat severe pain and joint damage.
- Assistive devices: Using assistive devices, such as knee braces or walking sticks, can help reduce joint stress and improve mobility.
Individualized treatment plans, often involving a combination of these approaches, are tailored to each individual’s specific needs and the severity of their knee arthritis. Regular communication with doctors is vital to monitor symptoms and adjust the treatment plan as needed.
Recovery
After any type of knee arthritis surgery, there is a recovery period. Recovery and recovery time depends on the type of surgery. Your doctor may recommend physical therapy to help you regain strength in your knee and restore range of motion. Depending on the procedure followed, you may need to use crutches or a cane for some time.
In most cases, surgery relieves pain and makes it possible to carry out daily activities more easily. These are only recommendations and may not apply to every situation.
- Category
- ΠΑΘΗΣΕΙΣ ΕΝΗΛΙΚΩΝ

